Abnormal wound healing: Clinic and treatment
Medical editor: Dr. Pierre Schneider, Dermatologist, Saint-Louis Hospital, France.
Related topics
- Scarring / Healing
Key messages:
- Healing of acute wounds is a physiological phenomenon which quality varies from one individual to another.
- The two main wound healing abnormalities are hypertrophic scars and keloids.
- Hypertrophic scars evolve favourably and regress over time, while keloids grow steadily and tend to recur.
- Compliance with the rules of initial wound management (cleaning, suturing, dressing) is the determining factor for a good quality scar, as aesthetically pleasing as possible.
- Keeping the scar moist and applying sun protection during the months following the injury are favourable factors in the evolution of the scar.
Acute wound healing is the sum of cellular and molecular mechanisms involved in restoring the anatomical and functional integrity of the skin barrier.
The normal wound healing process follows four main stages beginning immediately after the wound and continuing until complete healing4:
1. The coagulation and hemostasis phase
- A clot composed of fibrin, fibronectin, vitronectin, Von Willebrand factor (VWF) and thrombospondin-5, forms immediately after the injury.
- The clot interrupts bleeding while recruiting inflammatory cells that will ensure wound healing.
- The fibrin clot also provides a matrix substrate on which cells involved in wound healing can subsequently grow and multiply: neutrophils, macrophages, endothelial cells and fibroblasts.
2. The inflammatory phase
The inflammatory phase can be subdivided into 2 phases:
Early inflammatory phase
It begins at the end of the coagulation phase:
- Complement activation.
- Infiltration of polymorphonuclear neutrophils (PMNs) (24-36 hours after the wound) to prevent bacterial infection and destroy foreign particles and damaged tissue.
Late inflammatory phase (48h to 72h after the wound)
- Recruitment of macrophages to the wound healing site with chemoattractants (complement components, cytokines, elastin and collagen breakdown products).
- Macrophages are an important reservoir of growth factors and other cellular mediators and lead to the activation of keratinocytes, fibroblasts and endothelial cells.
- Lymphocyte recruitment at the wound healing site 72h post-injury.
3. The proliferative phase
It begins when the immune response is established, about 3 days post-injury and up to about 2 weeks afterwards. It is marked by:
- Proliferation followed by migration of fibroblasts and myofibroblasts, and synthesis of a new extracellular matrix.
- Synthesis of collagen I and III by the fibroblasts. The fibers are oriented parallel to the cutaneous tension lines.
- Angiogenesis from existing vessels and synthesis of granulation tissue
- Wound contraction by myofibroblasts allowing the two edges of the wound to be brought together.
4. The remodelling phase
- It can last up to 1 to 2 years.
- It corresponds to the remodelling of the granulation tissue by the action of collagenases and by the apoptosis of residual cells, as well as the deployment of a mature scar tissue.
- At the end of this remodelling phase, the scar is devoid of vessels, shows a decrease in local metabolic activity and a partial but incomplete restoration of its tensile strength (elasticity).
Healing is complete when the skin and other tissues involved in the injury have returned to their original anatomical appearance, function and structure.
- This process takes 5 to 10 days and can take up to 30 days in a non-pathological situation (outside the remodelling phase).
- Depending on the severity of the wound and individual factors such as age, general health, treatment and medical history, the healing process can be altered and result in poor quality or pathological scars.
Good to know:
Many factors, both local and systemic, can interfere with the normal course of wound healing5:
- Most common local factors:
- Poor circulation.
- Pressure sores.
- Poor wound cleaning (infection).
- Most common systemic factors:
- Age.
- Poor nutrition (obesity, malnutrition, deficiencies).
- Smoking.
- Terminal illness.
- Certain treatments (chemotherapy, immunosuppressants, corticosteroids, anti-coagulants).
- Certain chronic diseases (diabetes, rheumatoid arthritis in particular).
- The main abnormalities of acute wound healing are hypertrophic scars and keloid scars, each involving different molecular and cellular mechanisms.
- Both are nevertheless characterized by an excess of collagen production compared to normal skin: 7 times more collagen in hypertrophic scars, 20 times more in keloid scars6.
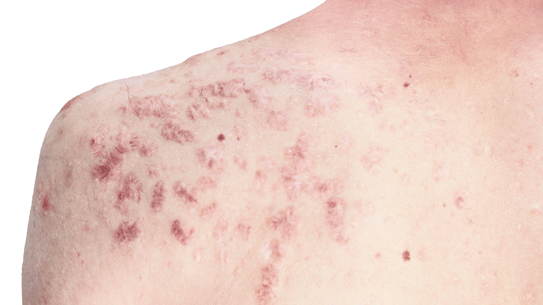
Hypertrophic scars
- Erythematous, pruritic lesions that form a bulge and remain confined to the lesion site1.
- Preferential areas of appearance: near joints or other stressed areas.
- Rapid development after the wound (4 to 12 weeks).
- Satisfactory evolution with progressive attenuation and flattening over time.
Keloid scars
- Keloid scars are more common in darker skinned individuals than in white skinned individuals.
- They protrude from the original wound site: scrapes, insect bites, vaccination shots, piercings, acne, surgical wounds or burns, usually in skin areas without hair follicles (neck, chest, shoulders, upper back, earlobes, abdomen).
- They can appear several years after the trauma and develop more slowly than hypertrophic scars.
- Unlike hypertrophic scars, keloids invade the surrounding skin and do not regress spontaneously.
- They frequently recur and can induce severe stress in the patient7.
Factors influencing wound healing
- The direction of the wound in relation to the skin tension lines (Langer lines): the orientation of the wound should be parallel to the Langer lines to achieve a good quality scar. Surgical wounds refer to these tension lines. Traumatic wounds perpendicular to these lines (especially at the level of a flexion fold) will systematically give a retractile scar.
- Wound site:
- Cursed areas: regardless of surgical technique, hypertrophic or keloid scars will usually be seen in the shoulder girdle, deltoid, pre-clavicular, and pre-sternal regions.
- Thin-skinned areas (eyelids): heal quickly with an excellent result unlike thick skin in seborrheic regions that heal poorly.
Preventative treatments8
In the months following wound closure:
Prevention of tension
- Especially on areas perpendicular to the Langer lines as well as on the shoulder and the presternal area.
- The application of strips or adhesive bands will limit the risk of abnormalities in the healing process.
Hydration and sun protection
- The healing process takes place in a moist environment.
- The use of emollients and silicones in sheets or gel is recommended.
- Sun protection (IF>50) is essential until the wound/suture has completely healed.
Compression
- With tailored garments in the initial phase.
- This approach concerns extensive scars (especially burns).
Curative treatments8
Intracicatricial injections of corticosteroids
- Anti-inflammatory and antifibrotic action, more effective on a young keloid or in the inflammatory phase.
- Effectiveness between 40 and 70%.
- The classic procedure consists of injecting corticoids directly and strictly into the scar (topical corticoids are only useful in case of pruritus).
- However, there are side effects inherent to the use of corticoids: skin atrophy, telangiectasias and pigmentation disorders if proper procedure is not respected.
Silicones
- Used in the form of plates, garments, gels in tubes or sprays on hypertrophic and keloid scars (burns in particular).
- Silicone gels probably act in a complex way on scars, notably by allowing hyperhydration of the corneal layer thanks to the occlusive effect created. They could also have an immunological action and participate in the restoration of a balance of the mechanisms involved in scar tissue remodeling.
- Specialized silicone plates and products require daily maintenance (washing in fresh water with neutral soap, followed by drying flat) and should not exceed approximately 30 days.
- Gel or spray silicones should be applied twice a day, whilst the scar is inflammatory and congestive.
- Silicones have few side effects and contraindications.
Cryotherapy
- Can be used as monotherapy or combined with intracicatricial corticosteroids.
- Frequent side effects: hypo- or hyperpigmentation, pain, atrophy.
- Cryotherapy is more effective on hypertrophic scars than on keloids.
- It can be used to cold burn residual keloids after reconstructive surgery.
- Advice on how to take care of a recent scar:
- Practice the palpate-roll technique on the scar.
- Apply compression bandages.
- Use healing creams.
- The patient must use photoprotection for at least 6 months to avoid secondary pigmentation.
- Inform the patient about the slow healing process leading to a positive outcome two years after the initial wound.
- There are risks involved when operating on a cursed area, where keloid scars are prone to develop.
- It is impossible to apply a simple surgical revision on a keloid scar.
Which dressings are suitable for covering a wound waiting to heal after suturing?
- Paraffin or silicone dressings should be used.
What are the pharmacological criteria of a healing cream?
- The pharmacological criteria of a healing cream are its emollient, anti-inflammatory, and antiseptic properties, as well as its ability to stimulate the synthesis of skin fibers (collagen, elastins).
In the case of umbilical cord scars: How long does the treatment last before the cord falls off?
- In general, about ten days.
What can be done in case of an abnormal umbilical cord healing?
- An abnormal umbilical cord scar often presents as a fleshy bud that can be treated with silver nitrate. However, if this bud persists, the new-born should be referred to be assessed for a possible fistula of the underlying umbilical cord. In this case, the bud is usually accompanied by oozing related to the fistula.
For caesarean scars: staples or sutures, is one method better than the other in terms of healing?
- Sutures are preferable as they produce nicer scars than staples.
When can palpate-roll be recommended on a Caesarean scar?
- Palpating and rolling can be recommended as soon as the threads are removed.
- Peacock Jr EE, Madden JW, Trier WC. Biologic basis for the treatment of keloids and hypertrophic scars. South Med J 1970;63(7):755–60.
- Bloemen MC, van der Veer WM, Ulrich MM, van Zuijlen PP, Niessen FB, Middelkoop E. Prevention and curative management of hypertrophic scar formation. Burns. 2009 Jun;35(4):463-75. doi: 10.1016/j.burns.2008.07.016. Epub 2008 Oct 31. PMID: 18951704.
- HAS-santé : Traitement des plaies par pression négative (TPN) : des utilisations spécifiques et limitées
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009 Sep-Oct;37(5):1528-42. doi: 10.1177/147323000903700531. PMID: 19930861.
- Enoch S, Leaper DJ. Basic Science of Wound Healing. Surgery (Oxford) 2008; 26(2):31-37.
- Karppinen SM, Heljasvaara R, Gullberg D, Tasanen K, Pihlajaniemi T. Toward understanding scarless skin wound healing and pathological scarring. F1000Res. 2019 Jun 5;8:F1000 Faculty Rev-787. doi: 10.12688/f1000research.18293.1. PMID: 31231509; PMCID: PMC6556993.
- Ojeh N, Bharatha A, Gaur U, Forde AL. Keloids: Current and emerging therapies. Scars Burn Heal. 2020 Aug 10;6:2059513120940499. doi: 10.1177/2059513120940499. PMID: 32844039; PMCID: PMC7418256.
- Meaume S. Le traitement médical des cicatrices hypertrophiques et chéloïdes, hors laser et thérapeutiques physiques - Doi : 10.1016/j.refrac.2018.07.009
Create easily your professional account
I create my account-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals