Pathologies of the Scalp: Clinic, diagnosis and treatment
Related topics
Key messages:
- All conditions affecting the scalp, meaning the skin of the skull and its hair system.
- Hair loss is a frequent reason for consultation in dermatology.
- In most cases, hair loss is not due to a medical condition (normal hair density depending on age, standard assessment showing no evidence of a pathology). However, this does not exclude the possibility of an emerging pathology requiring a follow-up assessment of the patient 3 to 6 months later.
- Conditions affecting the scalp are mostly diagnosed as diffuse or localized alopecia (hair loss).
- Scalp pathologies can also have symptoms of itching, dry skin patches, erythema, irritation and more.
- Scalp diseases include a wide range of other pathologies.
- Many factors can therefore come into play depending on the pathology: immunological, toxic, medicinal, traumatic, infectious, hormonal, localization of a general disease of the scalp or a specific scalp condition.
Circumscribed Non-Scarring Alopecia
Alopecia Areata
- It affects approximately 1 to 2% of the general population. However, the prevalence can vary between 0.1 and 6.9% depending on the population studied2.
- It mainly affects children (25%) and young adults, but all age groups can be affected1-3.
- Alopecia Areata is multifactorial, and the precise causes of its occurrence are still debated.
- However, genetic and immunological factors (autoimmunity) always seem to be involved1,2.
- Other factors such as oxidative stress, epigenetics or the intestinal microbiota could also play a role3.
Trichotillomania and Trichotemnomania1,4
- Trichotillomania is a form of obsessive-compulsive disorder. This condition mainly affects women (75%).
- Trichotemnomania refers to the cutting and/or shaving of hair in a manipulative and/or compulsive act. It often indicates an underlying psychological problem.
Fig: Trichotemnomania
Alopecia by Trauma and Traction1,5
- Ephemeral alopecia related to prolonged abusive hair pulling.
- It is often considered as affecting mainly people of African origin, however recent studies suggest that the main risk factor is not the type of hair but the maintenance habits.
Infectious and Inflammatory Alopecia1
-
- Any inflammation of the scalp can cause local hair loss (seborrheic dermatitis, shingles, insect bites).
- If it remains superficial, it is reversible.
- If it becomes chronic or deep, it can turn into scarring alopecia.
Alopecia in Clearings1
-
- Characterized by temporary alopecia.
- Occurs in 5% of cases following secondary syphilis.
Androgenetic Alopecia1,6
-
- Androgenetic alopecia (=baldness) affects 30% of Caucasian men in their 30s, 50% in their 50s and 80% in their 70s. It is also estimated that 30% of women are affected.
- Men of Asian or African origin seem to be less affected by this phenomenon.
- It is linked to two main factors: androgenic stimulation and genetics.
- One of the genes involved is carried by the X chromosome.
- This genetic background is associated with hair follicles (especially those on the top of the head) that are more sensitive to dihydrotestosterone, leading to an alteration in the hair renewal cycle: the cycle is accelerated and shortened, with early exhaustion of the number of cycles.
- Androgenetic alopecia also concerns women, in whom it can be triggered by oral contraceptives (pill) or hormonal treatments prescribed during menopause. Alopecia in women is also influenced by stress and excess cholesterol.
Diffuse Non-Scarring Alopecia
Telogen Effluvium1,7,8
-
- This is one of the most common causes of alopecia.
- Multiple factors can be at the origin of it: cerebral trauma, diet, childbirth, breast feeding, or medication.
Anagenic Effluvium (Dystrophic)1
-
- This is a sign of acute alteration of the anagen follicle which leads to dystrophy of the hair matrix, triggering hair loss by fracture of the hair shaft.
- It is distinguished from the telogen effluvium by a trichogram examination.
"Non-Alopectic" Alopecia1
-
- Some patients suffer from hair loss that cannot be linked to effluvium or alopecia.
- This is the case for dysmorphophobia or seasonal hair loss.
Scarring alopecia
This type of alopecia includes several pathologies, in particular specific scalp and hair follicle conditions (primary scarring alopecia), dermatoses with a particular localization (secondary scarring alopecia)1.
Inflammatory Scarring Alopecia
- Chronic lupus erythematosus.
- Lichen planus: in women over 30.
- Follicular degeneration syndrome: it never affects children and only rarely affects men.
Pustular Scarring Alopecia1
- Infectious Pustulosis:
- May develop following folliculitis.
- The search for infectious causes is very important.
- Quinquaud Folliculitis Decalvans:
- It is a chronic folliculitis.
- It affects both men and women.
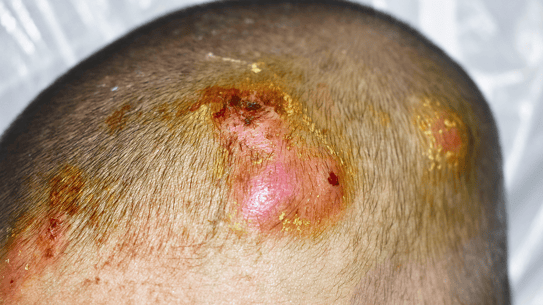
- Dissecting Cellulitis of the Scalp (DCS) (Perifolliculitis Capitis Abscedens, Suffodiens or Hoffman disease):
- May be associated with acne conglobata and hidrosadenitis suppurativa forming the acne triad.
- More often found in men.
- Tufted Folliculitis: affecting mainly people with black skin.
- Sterile Pustulosis: affecting the elderly.
- Quinquaud Folliculitis Decalvans:
- It is a chronic folliculitis.
- It affects both men and women.
- Dissecting Cellulitis of the Scalp (DCS) (Perifolliculitis Capitis Abscedens, Suffodiens or Hoffman disease):
- May be associated with acne conglobata and hidrosadenitis suppurativa forming the acne triad.
- More often found in men.
- Tufted Folliculitis: affecting mainly people with black skin.
- Sterile Pustulosis: affecting the elderly.
- Quinquaud Folliculitis Decalvans:
- It is a chronic folliculitis.
- It affects both men and women.
- Dissecting Cellulitis of the Scalp (DCS) (Perifolliculitis Capitis Abscedens, Suffodiens or Hoffman disease):
- May be associated with acne conglobata and hidrosadenitis suppurativa forming the acne triad.
- More often found in men.
- Tufted Folliculitis: affecting mainly people with black skin.
- Sterile Pustulosis: affecting the elderly.
Fig: Dissecting Cellulitis of the Scalp (DCS)
Non-Inflammatory Scarring Alopecia1
- Pseudopelade of Brocq: it mainly concerns women aged 25 to 45 years old.
- Fibrosing Frontal Alopecia: it is usually found in post-menopausal women but can affect men and women of all ages.
- Alopecia Musinosa.
Circumscribed Non-Scarring Alopecia1
Alopecia Areata1-3
- Manifested by spontaneous hair loss in a specific area (20% of cases) or in multiple areas.
- The areas are circumscribed, often circular. The size can vary, and the progression can be centrifugal (patchy alopecia).
- If the occipital region is affected, it is called ophiasic alopecia areata. This form is very resistant to treatment.
- In 5% of cases, the entire scalp can become bare, which is called alopecia totalis.
Fig: Alopecia totalis
- If the hair loss is diffuse (rare), it often progresses very quickly.
- In 10% of cases, nails may also be affected.
- The evolution of the disease is unpredictable, however, nearly 2/3 of patients recover spontaneously or respond to treatment.
- If the progression is rapid, if more than 25% of the scalp is affected, if the nails are affected or if the disease is ophiasic, then the prognosis is unfavorable.
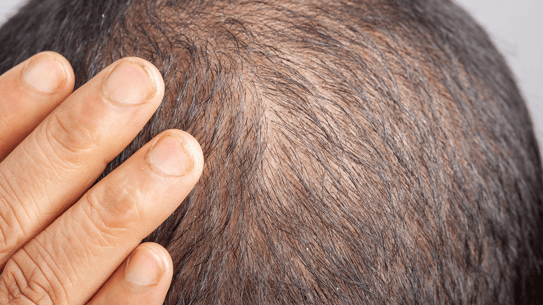
Androgenetic Alopecia1,6
- It is associated with diffuse hair loss.
- In men, it is associated with a symmetrical regression of the temporal edges until two bare gulfs are obtained. There is then a recession of the frontal border and a toning down of the top of the skull, which can be moderate or advanced. By progression and convergence, we obtain a Hippocratic baldness where only the temporal-occipital crown remains.
- In women, it is characterized by preservation of the temporal and frontal borders and occipital regions. There is an oval thinning of hair on the vertex and parietal region, rarely balding.
- The Ludwig scale details the stages of androgenetic alopecia.
Fig 1: Androgenetic Alopecia in men; Fig 2,3,4: Androgenetic Alopecia in women
Diffuse Non-Scarring Alopecia
Telogen Effluvium1,7,8
- It is very frequent.
- Various factors can interrupt the growth phase of hair (anagen phase) and cause it to enter a resting phase, which then results in delayed hair loss 3 to 4 months later, which can affect up to 50% of the hair mass.
- Spontaneous repair with return to a normal cycle takes 6 to 12 months.
Anagenic Effluvium (Dystrophic)1
- It is triggered by cytostatic drugs, the main ones being cyclophosphamide, docetaxel, paclitaxel.
- They cause a hair growth inhibition in the anagen phase resulting in a loss of all hair within 2 weeks following the first dose of treatment.
Scarring Alopecia
The pathological processes lead to the destruction of hair follicles, thus resulting in permanent alopecia. Treatments are generally not very effective1.
Inflammatory Scarring Alopecia
- Chronic Lupus Erythematosus (SLE):
- One or more large, erythematous, alopecic plaque covered with adherent scales, infiltrated at the edges and atrophic in the center.
- Sometimes painful or pruritic.
- Lichen Planus: in 50% of cases, other lichen localizations are found on the body, which confirms the diagnosis.
- Follicular Degeneration Syndrome:
- It starts in the center of the vertex and spreads slowly in a centrifugal manner.
- It may be inflammatory, accompanied by pustules or increased local sensitivity.
Pustular Scarring Alopecia1
- Quinquaud Folliculitis Decalvans:
- Presence of small, round, hairless patches dotted with pinhead follicular pustules.
- By progressive extension, linked to the confluence of the plaques, a vast atrophic area bordered by the active pustular lesions can be observed.
- Dissecting Cellulitis of the Scalp (DCS) (Perifolliculitis Capitis Abscedens, Suffodiens or Hoffman disease):
- Presence of large erythematous nodules evolving towards suppuration.
- The evolution is chronic.
- Tufted Folliculitis: it is characterized by the presence of tufts of hair emerging from a single orifice, resembling synthetic hair implants.
Non-Inflammatory Scarring Alopecia1
- Pseudopelade of Brocq: multiple, rounded or oval patches of smooth surface, small in size and then progressively spreading with the "appearance of footsteps in the snow".
- Fibrosing Frontal Alopecia (FFA): appearance of a smooth, symmetrical band of alopecia affecting the frontal region and the pre-auricular regions with progressive recession of the anterior hairline.
- Alopecia Mucinosa:
- The lesions are localized or diffuse.
- They are characterized by follicular keratotic papules.
- These papules are isolated or grouped in rather well-limited, erythematous plaques.
Diffuse Non-Scarring Alopecia1
- Target the etiology to eliminate the triggering drug or toxicant.
- Treatment of deficiencies: iron, zinc, vitamins, etc.
Androgenetic Alopecia9
- Male: finasteride 1mg/day taken orally and/or minoxidil 2 or 5% applied topically. Complementary hair transplant.
- Female: minoxidil 2% and 5% applied topically after menopause.
Alopecia1-3
- The first line of treatment is topical fluorinated corticosteroids. A monthly triamcinolone acetonide intradermal injection may also be considered, as it is more effective.
- These two treatments may be accompanied by 5% of minoxidil.
- The use of calcineurin inhibitors is not effective.
- If corticosteroids fail, immunotherapy can be prescribed by application of haptens to the scalp.
Scarring Alopecia
It requires specific targeted treatments administered in hospital.
Tips For Your Patients
Androgenetic Alopecia
- Fight against seborrhea of the scalp, an aggravating factor in alopecia.
- Do not hesitate to wash your hair every day with a mild, non-detergent, sulfate-free shampoo to avoid reactionary hyperseborrhea.
- Avoid drying hair at high temperatures, which promotes seborrhea.
Dandruff
-
Use an anti-dandruff shampoo, 3 times a week during the attack period, then once or twice a week for maintenance, alternating with a mild non-detergent shampoo.
-
Factors that irritate the scalp and aggravate dandruff should be avoided: blow-drying, brushing hair vigorously, hair coloring with ammonia, unsuitable detergent shampoos.
- Consult a dermatologist: They will be able to assess the scalp and find the dermatological signs leading to a diagnosis; they will carry out a secondary assessment and prescribe a relevant treatment.
- Reassure the patient:
- Regrowth will normally occur within 6 to 12 months in dermatoses with telogen effluvium or alopecia areata.
- A simple assessment is often sufficient to establish a diagnosis and lead to effective treatment.
- Explain:
- The patient's hair cycle and the normal, daily loss of 50 to 100 strands of hair which are naturally replaced. "We see the hair that fall out, but we don't see the hair that grows”.
- The need to limit aggressions on the hair (curling, perming, coloring, etc.) which lead to a fragility of the hair shaft and premature hair loss.
- In pediculosis, no treatment is 100% effective after one application, especially for nits, which requires repeating applications every 10 days (time it takes for the lice larvae to hatch). Nits can live for 10 days in the outside environment, so it is necessary to treat combs and caps, etc.
- Female or male androgenetic alopecia requires daily treatment to be continued over the long period of time (even in the case of hair transplants), because it only has an effect whilst being taken.
What type of shampoo can the patient use?
- In general, we recommend using a gentle shampoo for frequent use, 2 to 3 times a week depending on the level of seborrhea and possibly daily in the case of hyperseborrhea. Alternate with a specific care shampoo in case of seborrheic dermatitis.
Can alopecia be associated with grooves on the nail surface?
- Nail alterations, most often dystrophic, are indeed found in the context of alopecia totalis disease.
- Saurat J-H, Lachapelle J-M, Lipsker D, Thomas L. Dermatologie et infections sexuellement transmissibles. 5th edition. Masson, 2009.
- Juárez-Rendón KJ, Rivera Sánchez G, Reyes-López MÁ, García-Ortiz JE, Bocanegra-García V, Guardiola-Avila I et al. Alopecia Areata. Current situation and perspectives. Arch Argent Pediatr 2017; 115: e404–e411.
- Zhou C, Li X, Wang C, Zhang J. Alopecia Areata: an Update on Etiopathogenesis, Diagnosis, and Management. Clin Rev Allergy Immunol 2021; 61: 403–423.
- Melo DF, Lima C dos S, Piraccini BM, Tosti A. Trichotillomania: What Do We Know So Far? Skin Appendage Disord 2022; 8: 1–7.
- Pulickal JK, Kaliyadan F. Traction Alopecia. StatPearls Publishing, 2022 https://www.ncbi.nlm.nih.gov/books/NBK470434/
- Lolli F, Pallotti F, Rossi A, Fortuna MC, Caro G, Lenzi A et al. Androgenetic alopecia: a review. Endocrine 2017; 57: 9–17.
- Asghar F, Shamim N, Farooque U, Sheikh H, Aqeel R. Telogen Effluvium: A Review of the Literature. Cureus; 12: e8320.
- Rebora A. Telogen effluvium: a comprehensive review. Clin Cosmet Investig Dermatol 2019; 12: 583–590.
- Vidal. Quels sont les traitements de l'alopécie androgénétique ? [Accessed on 22/03/2023]
Create easily your professional account
I create my account-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals